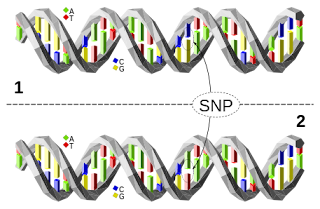
Detection of single nucleotide polymorphism (SNP)
by Steven Reehl, MBS 2020, GCSoM
Mentor: Michael Bordonaro, PhD
As medicine and healthcare have progressed throughout the decades, numerous changes have become apparent. These changes come in many forms regarding not only how we identify, treat, and manage disease, but what we identify, treat, and manage through our healthcare system. Along with this, the amount of money we spend on healthcare has changed drastically and likely will continue to. In developed countries, the prevalence of complex chronic conditions is only growing and so medicine has grown to meet this demand. Many chronic conditions are multifaceted, and it can be tricky to identify those at risk and then treat accordingly. Preventative care is a goal for the management of chronic conditions, but how can you prevent something that you aren’t capturing as a risk factor due to factors such as cost of screening.
A common risk factor for disease is a person’s genetics, or their underlying code. What is in in an individual’s genetic code has direct influence on their health. This means that, regardless of the environment that someone lives in, they may still develop a disease or condition if it is in their genetic code. This has huge implications for healthcare because we can control our environment and our lifestyle, but we mostly can’t control our genome. It is of the upmost importance that we can identify when our genetics put us at risk for a disease or condition.
One landmark that we can observe in our genome to identify an individual’s risk for disease is a single nucleotide polymorphism (SNP). These are distinct changes at a single location in someone’s genome and they account for about 90% of the variation between individuals. These SNPs can act as landmarks for disease. To put it simply, the presence of a certain SNP can indicate that someone has a higher risk for developing disease. Current methods of detecting SNPs that are associated with diseases are time consuming, expensive, and require specialized training. They do not lend themselves to being used as a reasonable screening method for disease. A reasonable solution to these problems must be found.
Lateral flow assays may offer the solution to proposed issues. A lateral flow assay is (typically) a paper-based device composed of several overlapping layers in series. Once you add a liquid sample to a lateral flow assay, it flows across the device without assistance. The device yields an easy to read signal, typically in the form of a color change. One of the most commonly known examples of a lateral flow assay is an over the counter pregnancy test. In the lab, lateral flow assays have been used for the detection of SNPs which are known to be associated with a disease phenylketonuria; a disease characterized by improper amino acid metabolism. The group of researchers was able to determine the presence of several different SNPs from a whole blood samples after processing by substituting a lateral flow assay for their detection method. They yielded accurate and sensitive results with their device, showing that lateral flow assays hold a reasonable place in the field of screening.
There are other examples of lateral flow assays being used as screening devices, but the results echo the same — they are the future. They offer an economical solution to an expensive problem. However, there is still a lot of work that needs to be done in order to use these devices in the clinic. The need for attention for these devices is necessary as research begins to summit their clinical potential. The potential they hold for screening is underscored by their potential to save money and lives in the long run. Lateral flow assays are the future for disease screening and disease detection, we need only harness their lightening in a clinical bottle.

Comments
Post a Comment